Call or Text
Call or Text
405-341-2062
Are You Sure You Don't Have Glaucoma?
Keeping with the theme of glaucoma awareness, this week’s Eye-Q blog is part two of our informative glaucoma run-down where we will be covering the symptoms of glaucoma, as well as information on how it is diagnosed and some of the common treatment options. If you haven’t yet checked out part one to find out what exactly glaucoma is (including the different types of glaucoma) and what your risk factors are for developing the sight stealing disease, you can read it here.
Ok, let’s get started.
The Silent Sight Stealer
Unfortunately one of the factors that makes glaucoma such a threat is that it often has no symptoms at all until the disease has progressed and vision is lost. This is why early detection through a yearly eye health exam is so important - especially if you have any of the related risk factors.
Primary Open Angle Glaucoma (POAG) - No symptoms typically present.
Low Tension Glaucoma - No symptoms typically present.
Angle Closure Glaucoma - Angle closure glaucoma is one of the only types of glaucoma that will exhibit symptoms. These can include sudden onset eye pain, hazy or blurred vision, rainbow colored circles around bright lights, nausea or vomiting, and sight loss. It is important to seek immediate medical care if these symptoms are suddenly experienced.
Childhood Glaucoma - Much like adult glaucoma, juvenile glaucoma will usually develop without any obvious symptoms. However, a few things you can look for are a cloudy appearance to the eye (s), an abnormal enlargement of the eye(s), and some systemic symptoms such as loss of appetite, vomiting, and irritability.
How Is Glaucoma Diagnosed?
By now you might be wondering how in the world glaucoma is diagnosed if there aren’t even any symptoms. Again, the key is early detection through yearly eye health exams. Your eye doctor can detect glaucoma or even an increased risk for glaucoma long before any damage is done to your sight. The importance of this truly can’t be stressed enough because once your vision is gone, it can’t be restored. Here are a few of the common tests performed together with a comprehensive eye examination to help your optometrist determine if you have glaucoma or are at an increased risk for developing the disease.
Imaging Technology - There are now a number of advanced imaging systems available to assist your optometrist in evaluating the optic nerve and retinal nerve fiber layer (these are the areas commonly damaged by glaucoma). These devices include laser polarimetry, scanning laser tomography, and ocular coherence tomography (OCT). Photographs of the optic nerve are also extremely useful in documenting changes over time that could signal damage or the onset of glaucoma as well as other systemic or eye health conditions.
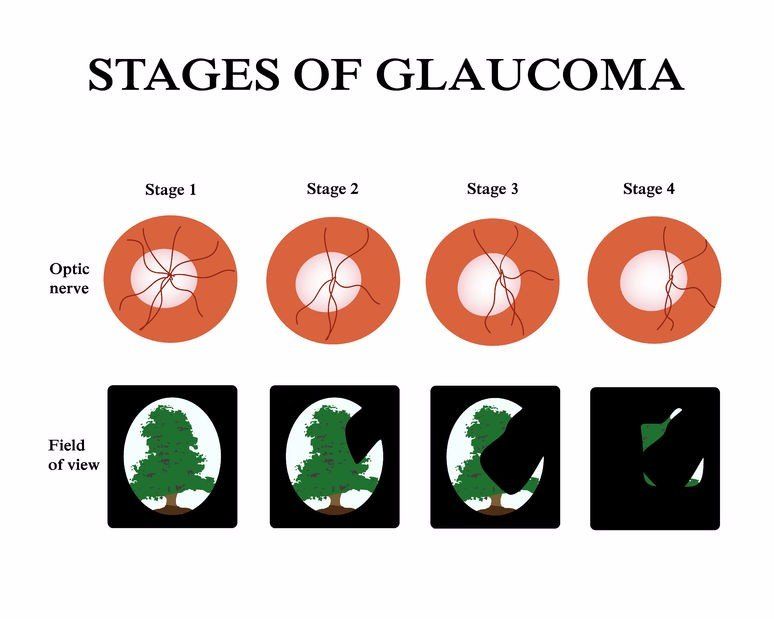
Visual Field Testing - As the name would suggest, this offers your doctor a detailed view of your field of vision - focusing primarily on your peripheral vision (aka side vision). This is important in glaucoma because your peripheral vision is most commonly affected first. However, this loss is typically so faint initially that most people do not even notice the visual decrease until it moves farther in centrally.
Tonometry - So far we have mentioned the eye’s intraocular pressure (IOP) a few times as an important factor in diagnosing and managing glaucoma. A tonometer is the device used to measure and calculate this value. There are several different kinds of tonometers including the infamous NCT (non-contact tonometry) machine better known to most as the “puff-of-air” test.
Pachymetry - This is a quick and painless measurement of how thick or thin the cornea (front surface of the eye) is. This is helpful because if a person has particularly thick corneas, their IOP will appear to be higher than it actually is. Having the most accurate IOP measurement possible is important in obtaining a diagnosis of glaucoma as well as in managing and treating the disease.
Gonioscopy - Gonioscopy allows your optometrist to view the angle between the iris and cornea where fluid drains from the eye with the use of a handheld mirrored lens. This lens shows the doctor if the angle is wide open or narrow. Narrow angles increase an individual's risk for a sudden acute glaucoma attack. Furthermore, gonioscopy can also determine if there are any blockages in the drainage canal such as abnormal vessel growth or excessive pigment.
Treatment Options
While glaucoma can be an aggressive and potentially devastating eye disease, the good news is - it doesn’t have to be. If detected early and properly managed, most people will not have to go through losing their sight. Luckily there are several different options for treatment depending on the type of glaucoma you have and how advanced it is.
Eye Drops - Eye drops are primarily used to help lower the eye’s IOP by decreasing the amount of fluid made by the eye and/ or helping the eye’s fluid to drain more effectively. There are a number of drops available to treat glaucoma and each is classified by their active ingredient. There are also combination drops available for those who need more than one type of medication.
Pills - When eye drops alone are not able to efficiently control IOP, oral medications might be added to your regimen. Oral glaucoma medications have the same purpose as eye drops - to lessen the production of fluid within the eye.
Laser Surgery - There are actually several different kinds of laser surgeries used to treat glaucoma depending on the type of glaucoma you have as well as the severity. The most commonly performed treatment is called a trabeculoplasty. This is a quick and painless procedure in which a high energy light beam is focused on the eye’s drainage system and makes subtle changes that allow the aqueous fluid to drain more efficiently.
Traditional Surgery - In more advanced glaucoma when medications and/or laser treatments are not able to lower eye pressure adequately, conventional surgery might be recommended. The most commonly performed procedure is called trabeculectomy. During this surgery, a passage is created in the sclera (the white of the eye) that allows excess fluid to drain freely.
Regardless of the method - the goal of any treatment is to prevent the loss of vision. It is extremely important to stay on top of taking medications as prescribed and keeping your follow up appointments to see your doctor.
Visit the Glaucoma Research Foundation ’s website for a more comprehensive list and further explanation of both surgical and non-surgical treatment options. Also be sure to stay tuned for our final glaucoma awareness post to find out some surprising statistics as well as ways you can help keep others from getting blind sided by glaucoma.
Our Culture
AMD Center of Excellence
Hours
| Monday | 7:30am-6:00pm |
| Tuesday | 7:30am-6:00pm |
| Wednesday | 7:30am-6:00pm |
| Thursday | 7:30am-6:00pm |
| Friday | Closed Most Fridays |
Our Culture
AMD Center of Excellence
Hours
| Monday | 7:30am-6:00pm |
| Tuesday | 7:30am-6:00pm |
| Wednesday | 7:30am-6:00pm |
| Thursday | 7:30am-6:00pm |
| Friday | Closed Most Fridays |